The post Joint session tackles SPARC, APCCC disparities, and a new RCC tracer appeared first on EMUC25.
]]>SPARC the conversation
In “SPARC initiative: The final consensus”, Dr. Jochen Walz (FR) emphasised, “PSMA theranostics in PCa is here to stay. Several publications have shown the benefits of using PSMA technology to improve the management of our patients. What we lack is a common language.” According to Dr. Walz, there is an absence of standardised and accepted reporting of PSMA-PET. Clear and standardised communication between nuclear medicine physicians and clinicians (e.g., urologists, medical oncologists, radiotherapists, etc.) is essential
“The summary of the consensus we generated and the reporting standards established concerning detection (i.e., looking for PCa in a patient that was not yet diagnosed with PCa similar to what mpMRI is doing nowadays) is that MRI is not first-line for detection. There might be cases of inconclusive MRI, the same with biopsy findings. Added information might be of value,” said Dr. Walz. He underscored that a biopsy is still necessary, “even if it is PI-RADS 5, SUV > 12; even if MRI and PSMA-PET results are negative, but there is a strong suspicion that the patient has PCa.”
Dr. Walz also provided the consensus on the standards of PSMA-PET reporting on primary staging, biochemical recurrence, and treatment response.
APCCC diagnostics disparities
In the first part of the presentation, “APCCC diagnostics: Agreements and disagreements”, medical oncologist Dr. Fabio Turco (CH) provided the aims of the APCCC, such as:
- Gather recommendations on managing advanced PCa, especially in areas where evidence is scarce or conflicting, or if there is a different interpretation of evidence
- Knowledge translation
- Identify knowledge gaps
Prof. Goffin then discussed the APCCC Diagnostics 2025, which comprised 88 questions divided into six categories: how to diagnose PCa; how to stage PCa; biochemical recurrence; metastatic disease: What to do; monitoring metastatic PCa; and radioligand therapy and imaging. Prof. Goffin also shared some of the questions which resulted in disparities among recommendations. The APCCC Diagnostics 2025 paper is ongoing. The call for abstracts deadline is 23 November 2025.
Renewed interest in tracers
In his presentation “Advances in molecular imaging in renal cancer”, nuclear medicine physician Dr. Clément Bailly (FR) stated that there is limited performance of tracers in nuclear medicine for the diagnosis of kidney cancer, but there is renewed interest tracers, particularly in theranostics. He focused on Carbonic Anhydrase IX (CA IX), which is a cell-surface glycoprotein that contributes to pH regulation. He stated that CA IX expression in non-cancerous tissues is rare and generally confined to the epithelia of the stomach, gallbladder, pancreas, and intestine. The expression is notably induced by hypoxia, and is notably induced as a consequence of the inactivating mutation of the pHVL tumour suppressor protein.
(Re)watch the full presentations via the EMUC25 Resource Centre.
The post Joint session tackles SPARC, APCCC disparities, and a new RCC tracer appeared first on EMUC25.
]]>The post PSMA PET/CT: Prime tool in staging and treatment monitoring appeared first on EMUC25.
]]>In his pre-recorded lecture “Optimal staging approach in men recurring after primary treatment”, Prof. Declan Murphy (AU) stated, “There is no role for imaging in patients with PSA > 0.2 ng/mL detectable on an ultrasensitive assay.”
He cited three publications (1) which confirmed that the cancer benefit of waiting for PSA to reach 0.2 ng/mL first and then offering salvage radiotherapy is as good as providing adjuvant radiotherapy when the PSA is below 0.2 ng/mL. Moreover, it is less toxic and overtreatment can be avoided. He added that imaging may have a role within the range of 0.2 ng/mL up to about 2 ng/mL.
According to Prof. Murphy, conventional imaging such as CT and bone scan is pointless in these low-range settings. “Please don’t do a CT and bone scan when the PSA climbs above 0.2 ng/mL even just to reassure your anxious patients. MRI has a role for staging loco-regional recurrence especially if novel imaging is unavailable.”
He underscored that PSMA PET/CT is the best imaging tool for biochemical recurrence as it is the most sensitive and the most specific imaging modality for biochemical recurrence for PCA patients. “Use PSMA PET/CT once the PSA is above 0.2 ng/mL as it may change your management.”
Prof. Murphy referred back to the findings of the aforementioned three publications (1) which collectively substantiated that PSMA PET/CT has an impressive sensitivity for detecting disease in men with biochemical recurrence even at very low PSA levels of < 1 ng/mL with specificity well above 90%. He added, “PSMA PET/CT offers a safe, one-stop whole-body scan with excellent tumour-to-background-contrast ratio.”
Treatment monitoring
Following Prof. Murphy’s presentation was the lecture of radiologist Dr. Ekaterini Tavermaraki (GR) entitled “How to use imaging for treatment monitoring in metastatic prostate cancer”.
Dr. Tavermaraki stated that conventional imaging still has a role in the follow-up of patients under systemic treatment. She added that modern PSMA PET/CT imaging techniques provide better sensitivity and specificity for metastases detection, especially in biochemical recurrence in low values of PSA. Subcentimeter-target lesions which are not measurable at CT, are visualized. PSMA PET/CT imaging provides earlier response information than anatomic imaging methods.
She also mentioned the pitfalls of PSMA PET/CT which include low to moderate PSMA expression in osteoblastic activity, moderate uptake in haemangiomas, and chronic inflammation can also be associated with PSMA uptake. She stated, “All of these cases correlate with anatomic findings. If there is uncertainty, ongoing monitoring of the PSA level with follow-up PSMA PET is suggested.”
In addition, the limitation of PSMA PET/CT is that if the primary tumour is not PSMA-avid, the sensitivity for detecting nodal or distant metastatic disease will be lower, and closer attention must be given to anatomic review.
Watch the full presentations of Prof. Murphy and Dr. Tavermaraki and other must-view presentations of Plenary Session 1 via the Resource Centre.
References:
- Gallium-68 Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer-Updated Diagnostic Utility, Sensitivity, Specificity, and Distribution of Prostate-specific Membrane Antigen-avid Lesions: A Systematic Review and Meta-analysis (Perrera et al, Eur Urol 2020)
- Assessment of 68Ga-PSMA-11 PET Accuracy in Localizing Recurrent Prostate Cancer: A Prospective Single-Arm Clinical Trial (Fendler, Calais, Eiber, et al., JAMA Oncol 2019)
- Diagnostic Performance of 18F-DCFPyL-PET/CT in Men with Biochemically Recurrent Prostate Cancer: Results from the CONDOR Phase III, Multicenter Study (Morris et al., Clin Can Res 2021)
The post PSMA PET/CT: Prime tool in staging and treatment monitoring appeared first on EMUC25.
]]>The post Strengths and limitations of PSMA PET: When to use it (and when not to) appeared first on EMUC25.
]]>Nuclear medicine physician Dr. Fanti kicked off the session with his state-of-the-art lecture “Strengths and limitations of PSMA PET for primary staging.” “To every extent, PSMA PET has been a gamechanger,” Dr. Fanti said. “Today, PSMA PET is widely used in many situations all around the world.”
“As for the use of PSMA PET in PCa staging, some papers really made a difference. One of those was an Australian prospective, randomised, multicentre study, which clearly demonstrated that PSMA PET was superior to conventional imaging in patients with high-risk PCa.”
“The 2022 EAU Guidelines on Prostate Cancer will recommend using PSMA PET or a whole-body MRI in high-risk patients to increase the sensitivity,” Dr. Fanti continued. “The guidelines will emphasise the very important limit of the lack of outcome data on subsequent treatment changes. PSMA PET is more accurate than CT and a bone scan, but we don’t know if there will be an impact on overall survival. And we know that a better accuracy does not necessarily mean better outcomes. Having said that, there’s a strong rationale behind using PSMA PET in patients with high-risk disease.”
Dr. Fanti concluded, “PSMA PET is a robust imaging methodology, non-invasive and patient-friendly, with a clear procedure and a wide availability worldwide. It will have a further role in staging high-risk patients.”
Debate
In the following debate, Prof. Maurer and Dr. Walz answered the question of whether PSMA PET should have an impact on the treatment of newly diagnosed PCa: yes (Prof. Maurer) or no (Dr. Walz).
Prof. Maurer asked his audience, “Do we know whether PSMA PET leads to better outcomes? Most of you will say, ‘We don’t know that,’ and for the most part that’s true. But I will show you a specific scenario in which I believe PSMA PET already makes a difference today.” He went on presenting the slide below.
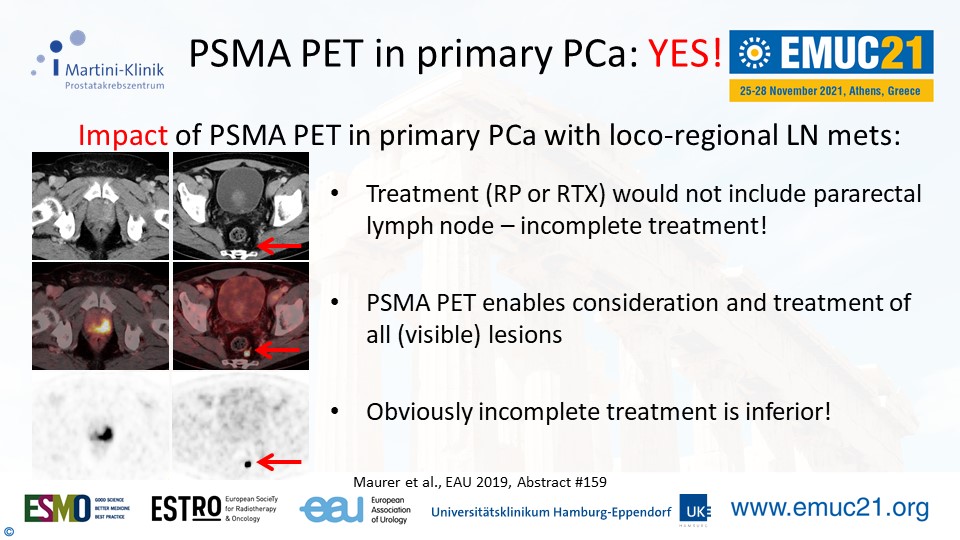
“My recommendation is to consider PSMA PET in the cases of unfavourable intermediate and high-risk PCa. Certainly there are still a lot of unanswered questions. But we, and our patients, now have an imaging tool that helps us better understand the disease state. So PSMA PET for primary PCa? Yes, please!”
Dr. Walz’ presentation followed right after. He said, “The difference between PSMA and conventional imaging is that the former’s increased sensitivity detects especially lymph node metastases. But what is the consequence of this increased sensitivity?”
“Should we abandon local treatment in ciM0/miM1? Provide systemic treatment only? Disregard the information gained from PSMA? Choose local, systemic, and metastases-directed treatment? So far we don’t know.”
He concluded his presentation with a quote from Prof. Henk Van Der Poel (NL), who was attending the presentation. “Care should be taken to avoid unproven treatment decisions that may result in undertreatment [or overtreatment] and finally harm to patients.”
Get the full perspective from both sides by (re)watching the presentations. EMUC21 delegates can access all scientific content in the EMUC21 Resource Centre. All presentations, full-text abstracts, and (e-)posters will become easily accessible here during the congress.
The post Strengths and limitations of PSMA PET: When to use it (and when not to) appeared first on EMUC25.
]]>The post Imaging and pathology: The harm of false positives appeared first on EMUC25.
]]>The speakers gave several examples of mimicking of PCa or of bone metastasis, or the grey areas within a PI-RADS scoring. Their talks gave the assembled urologists and oncology specialists a good idea of the possible false positives that have to be ruled out before any conclusions can be drawn from imaging or pathology. Following the session, we spoke to Prof. Thoeny about the topic, particularly what specialists can and should do in the case of a false positive.
Always consider the complete picture
Prof. Thoeny recommends looking at the whole history. “When it comes to PCa, always look at the morphology. But also the available clinical data, like the PSA. If there is a discrepancy (for instance a low PSA but a lot of metastasis), if there is a minimal doubt, you have to perform a biopsy to prove your theory. Chemo and hormone therapy have a huge impact on the patient and should be avoided if possible.”
“It is very difficult to draw conclusions on metastasis based PSMA-PET. I know that there is a lot of enthusiasm for the technology and it is sometimes considered to be the holy grail, but it’s not.”
Is imaging only suitable in combination with other methods? “No, I think MRI of the prostate, this is the way to go,” said Thoeny. “Of course you need extra training but I agree…”
The PI-RADS scale of course also has scope for false positives. “The difficult ones are PI-RADS 3, because you’re not sure how to proceed. Taking the PSA density into account can help you rule out false positives. There are plenty of calculators online. There is a cut-off of 0.12ng/ml. If it’s higher than 0.12, then it’s more aggressive, and if it’s lower we do a follow-up.”
A friend of a friend
Prof. Thoeny related a recent case she was involved in around two years ago, a friend of a friend in his early 50s. “His Gleason score was determined to be 6-8 following a biopsy. He went to have a PSMA-PET done. I hadn’t heard from him in a while. He later told me that he was told that he had bone metastasis and lymph node metastasis. They had said ‘Surgery can’t help you. You will get hormonal and radiotherapy, and possibly chemo. You have another 3-4 years left to live.’ He was in an intense shock. He walked out of the clinic and thought to himself: ‘I hope I’ll have a car accident,’ he didn’t want to live anymore.”
“The specialists had looked at morphology, and it looked really suspicious on the images. This seemed odd to me, considering that he had a stable PSA for 5 years. I asked him to send me all the images of the previous years. I went back and looked at the old MRIs, and you could tell that the bone lesions were there already 5 years ago. I told him: undergo surgery, have a lymph node dissection done. They were all negative. He’s now happy and in good shape.”
“We have no idea what caused the false positive, it’s still a mystery. There’s a lesson for today’s audience: if the whole story doesn’t fit together, you should be more critical. In the case of PSMA-PET, you should have a biopsy for confirmation before undergoing the extremely impactful systematic treatments. In the case of a prostate MRI, if you take PSA density into account, follow-up should be enough.”
The post Imaging and pathology: The harm of false positives appeared first on EMUC25.
]]>