The post 2023 ends with big game changers for GU cancers appeared first on EMUC25.
]]>Urologist Ms. Maxine Tran (GB) delivered a presentation on ‘Nephron Sparing Treatment (NEST) for small renal masses’, a feasibility study of a cohort embedded randomised controlled trial comparing nephron sparing treatment for small renal masses.
Ms. Tran stated that feasibility of the trial was demonstrated, intervention was acceptable (85%), there were fewer complications, less reduction in renal function, reduced hospital stays, decrease in costs, and intervention showed equivalent cancer control.
In his presentation, ‘Update on PSMA targeting’, Dr. Andrea Farolfi (IT) shared results and comparisons of the PSMAfore (phase 3) and ENZA-p (phase 2) trials.
Dr. Farolfi: “PSMA-targeted radioligand therapy (RLT) is gaining momentum globally and there are new trials coming. Lutetium PSMA is quite active in this taxane-naïve metastatic castration-resistant prostate cancer (CRPC) space, and was extremely well tolerated. We have a new therapy that eventually, when regulators approve, will be available for patients in this space.”
“We do not need to sacrifice the quality of life (QoL) for oncological benefits. Enzalutamide combination and enzalutamide monotherapy do not negatively affect health-related quality of life (HRQoL),” stated Prof. Stephen Freedland (US) in his presentation on the EMBARK trial.
According to Prof. Freedland, in patients with high-risk biochemical recurrence (BCR) compared with leuprolide acetate, the enzalutamide combination demonstrated a statistically significant and clinically meaningful improvement in metastasis-free survival (MFS) (HR 0.42; 95% CI, 0.30-61; P<0.0001).
“Enzalutamide monotherapy also demonstrated statistically significant and clinically meaningful improvements in MFS (HR 0.63; 95%, CI 0.46-0.87; P=0.0049), time to PSA progression, and time to the first new antineoplastic therapy. No new safety signals observed to date with enzalutamide treatment”.
“Enzalutamide in combination with androgen deprivation therapy (ADT), if approved in this setting, has the potential to become a new standard of care for patients with high-risk BCR (biochemical recurrence).”
In her lecture, ‘Update on TALAPRO and PROpel’, medical oncologist Dr. Friederike Schlürmann (FR) shared a summary of game-changing improvements in overall survival (OS) over the years with the addition of PARPi to ADT+ARSI (androgen receptor signalling agent) in metastatic castration-resistant prostate cancer (mCRPC).
Dr. Schlürmann: “The TALAPRO and PROpel trials show clinical benefit beyond HRRm, and all trials support activity for PARPi + NHA in HRRm/BRCAm mCRPC. There must be caution with cross-trial comparison and differences in the study designs, populations and dosing schedules between trials may provide considerations for the differences seen between trials.”
On the topic of testing, Dr. Schlürmann stressed that somatic testing for BRCA1/2 has to become the standard of care in PCa.
Great news for BCa patients
Prof. Tom Powles (GB) was beamed in from America to deliver a presentation on the EVO-302/KEYNOTE-A39 trial. “This is the first time that platinum-based chemotherapy has been surpassed in OS in patients with previously untreated locally advanced/metastatic urothelial carcinoma (la/mUC). The overall results support enfortumab vedotin plus pembrolizumab (EV+P) as a potential new standard of care for 1L la/mUC.”
According to Prof. Powles, EV+P showed statistically significant and clinically meaningful improvement in efficacy over chemotherapy with a progression-free survival (PFS) of HR 0.45 and OS was 0.47%. Median PFS (mPFS) and median OS (mOS) were nearly doubled in the EV+P arm compared with chemotherapy. The benefit in prespecified subgroups and stratification factors were consistent with the overall population. The safety profile aligned with expectations and no new safety signals observed. EV treatment-related adverse events of note were skin reactions, peripheral neuropathy and sensory events.
Dr. Yohann Loriot (FR) presented on the THOR trial, stating that in the trial that erdafitnib significantly extended the OS in patients with advanced/mUC with FGFRalt after prior treatment with anti-PD-(1), with a mOS of 1 year.
According to Dr. Loriot, erdafitnib provided a 36% reduction in risk of death compared to chemotherapy, the OS benefit of erdafitnib was consistent across the relevant subgroups, and it offered significantly longer PFS and greater objective response rate (ORR) compared to chemotherapy.
Dr. Loriot: “This phase 3 THOR study supports the clinical efficacy of erdafitnib as the standard of care option for patients with mUC with FGFRalt after anti-PD-(L) 1 treatment, and the OS benefit of erdafitnib in patients with mUC with FGFRalt supports molecular testing for FGFRalt in all patients with mUC”.
You can watch a webcast recording of the full presentations on the EMUC23 Resource Centre.
The post 2023 ends with big game changers for GU cancers appeared first on EMUC25.
]]>The post “If you can’t measure it, you can’t improve it” appeared first on EMUC25.
]]>Mr. Leigh: “We will consider three cases in this session, using the format of an M&M Meeting. We will try to be candid and fair, looking for ways to improve practice. We asked our presenters to choose cases from which lessons may be learned. None of the cases have obvious negligence, but all present learning opportunities.”
A quality audit – measuring outcomes and complications
Asst. Prof. Giorgio Gandaglia (IT) presented a prostate cancer case from his institution for review.
- A 72-year-old male
- BMI 23
- Type 2 DM
- Medication: metformin
- PSA 4.3 ng/ml
- CT scan: prostate x 1.5, suspicious module right side, prostate 40ml; adenoma 20 ml, prostate biopsy showed adenocarcinoma of the prostate, FF2, 5/15 positive cores, bone scan was negative, abdominal TC: bilateral renal cysts
The patient underwent a robot-assisted radical prostatectomy. He was discharged on day three postoperative, but on day six, he was admitted to the ER with haematuria and fever, a malfunctioning of the bladder catheter. He was re-admitted to the ER on day 30 with the same complication.
Is it important to chase complications after robotic surgery? According to Asst. Prof. Gandaglia, a wide heterogeneity exists in the rate of postoperative complications after robotic surgery. Although, there has been an exponential increase in the papers using the Clavien-Dondo system over the last few years, only 65% of urologic manuscripts adopt the score correctly.
Asst. Prof. Gandaglia shared details on how his institution learnt from this experience. “The first phase of our prospective study consisted of an audit and feedback process, where the most frequent complications observed in our series were prospectively collected, and in January 2018 an appraisal was done. The most common complication was anastomotic leaks (6.7%). Changes in the surgical technique were proposed to improve outcomes after collegial discussion and review of the surgical videos were recorded during the audit and feedback phase.”
According to Asst. Prof. Gandaglia, the outcome was the introduction of a novel technique for vesico-urethral anastomosis. “The awareness of postoperative outcomes led to the implementation of changes in the surgical techniques that significantly reduced the risk of specific postoperative complications.”
Risks of radical cystectomy
Dr. Carmen Mir (ES) presented a bladder cancer case and how the outcome led to learning and making changes to limit the chance of surgical site infections. She stated that reviewing the risks of radical cystectomy need to cover interoperative, in-hospital, early recovery, and long term. Changes implemented in her institution from this case included fragility assessment for patients over 70 years old, redoes antibiotic therapy and the use of chlorhexidine for prepping. “We also change the surgical instrument set at closure, use running 5mm 1-0 resorbable elastic monofilament, and saline for wound clean up before skin closure”.
A take-home message from Dr. Mir was “Look at your own institution and see what is working and what’s not working. There are a lot of small things that could make a difference to the outcome”.
A need for anticoagulation therapy (ACT) pre-operatively?
Prof. Faiz Mumtas (GB) presented a complicated kidney cancer case of an 80-year-old male with a high BMI of 38 and a visible haematuria with a normal MSU, blood profile and cystoscopy. He had a permanent pacemaker for asymptomatic bradycardia.
According to Prof. Mumtas, in the patients initial CT scan he had a level 2 Pt3b caval tumour. “His staging CT and MRV (Magnetic Resonance Venography) got delayed whilst waiting for a cystoscopy and so he represented with a saddle pulmonary embolism (PE) with an extension in the caval tumour height. With extensive PE we did anticoagulated therapeutically with no significant haemodynamic improvement. Surgery was delayed due to recurrent PE. This further delay led to the growth of the tumour size and it now approached the level of the hepatic veins making it level 3. This indicated a significant progression.”
Prof. Mumtas stated that a cardiac bypass had to be performed at a different institution. He concluded his presentations with the learning points from this case:
- Anticoagulation in the presence of high-risk factors – recurrent VTE (venous thromboembolism) and bland tumours
- Concerning up-to-date imaging, Prof. Mumtas suggests no more than a couple of days before surgery.
- Further multicentre studies are needed to explore the role of pre-operative anticoagulation and neoadjuvant systemic treatments.
- Operating on level 3 tumours only in facilities where cardiac bypass is available, is to manage patients who become haemodynamically unstable with supra-hepatic clamp.
You can watch a webcast recording of the full presentations on the EMUC23 Resource Centre.
The post “If you can’t measure it, you can’t improve it” appeared first on EMUC25.
]]>The post What’s new in GU Pathology and WHO classification? appeared first on EMUC25.
]]>In her lecture “The new WHO classification of renal tumours”, Pathologist Dr. Maria Rosaria Raspollini (IT) shared an update on the 2022 classification changes, addressing the concept of molecularly defined renal tumour entities in particular. According to Dr. Raspollini, traditionally, renal tumour subtypes have been named on the basis of predominant cytoplasmic features (clear cells/pink cells RCC) and chromophobe RCC. Now there are renal tumour subtypes named on the basis of architectural features (papillae RCC).
Dr. Raspollini stated: “Clear cell RCC account for 60-75% of all RCC’s and are characterised by neoplastic cells with predominantly clear and occasionally eosinophilic cytoplasm, accompanied by an abundant network of blood vessels and associated with biallelic VHL inactivation. Chromophobe RCC accounts for 5-7% of cases and are characterised by large pale and/or smaller eosinophilic tumour cells with wrinkled nuclei and perinuclear haloes. The WHO 2022 papillary RCC is characterised by papillary and tubular structures lined by cuboidal cells with scant or lightly basophilic cytoplasm with an overall basophilic appearance. Foamy histiocytes and psammoma bodies may also be present.”
On the topic of new renal tumour entities, Dr. Raspollini stated that clear cell papillary renal cell carcinoma has been reclassified as clear papillary renal cell tumour, because there is not a described metastatic event. “These tumours are mainly pT1 well-circumscribed, encapsulated and cystic change can occur. Specific molecular pathological features that it lacked were chromosome 3p loss and alterations of VHL, as well as mutations in TSC1, TSC2, MTOR or ELOC (TCBE1).”
According to Dr. Raspollini, another new entity is Eosinophilic solid and cystic renal cell carcinoma (ESC-RCC). “These are typically well-circumscribed, tan, solid and cystic, with reported sizes ranging from <10 to 135mm. ESC-RCC is characterised by solid and cystic architecture, eosinophilic cytoplasm and coarsely granular, basophilic cytoplasmic stippling. The majority of ESC-RCC’s appear to have been cured by resection. Rare cases with metastases have been reported.”
Morphological and molecular reporting strategy
During his lecture “The new WHO classification of bladder tumours – why the morphology is important in the molecular age”, Prof. Antonio Lopez-Beltran (PT) shared details on non-invasive urothelial neoplasms, points of practice and novelties, including urothelial papilloma and inverted urothelial papilloma.
“The classification papillary urothelial hyperplasia has disappeared” stated Prof. Lopez-Beltran. “We should report cases even if the WHO does not recognise it”.
Prof. Lopez-Beltran questions the correctness of the newly classified urothelial carcinoma “subtypes”, which were previously “variants”. The term “variant” has been exclusively reserved for genomic alternations. In his opinion, they are genetic variations.
Looking at what lies ahead in the future, Prof. Lopez-Beltran voiced the proposal of a combined morphological and molecular reporting strategy. “This is an evolving process from WHO in 1973 to WHO 2002/2016 to molecular subtyping using immunohistochemistry. Advantages of combined reports include providing the clinician with more information sooner, leading ultimately to a more personalised approach to current therapies.”
Prof. Lopez-Beltran ended his lecture with the comment “classifications are getting more difficult and more complicated, but we need to tell clinicians that we are going forward. We are driving towards a new time for pathology”.
The post What’s new in GU Pathology and WHO classification? appeared first on EMUC25.
]]>The post EMUC22 Preview: “Treatment intensification in mHSPC is a hot topic right now” appeared first on EMUC25.
]]>In this article, world-renowned cancer researcher and EMUC22 Steering Committee member Prof. Silke Gillessen (CH) shares her personal programme highlights in an interview about the upcoming congress.
In your expert opinion, what are the most relevant topics at EMUC22 and why?
Prof. Gillessen: This is difficult to decide because they are all relevant, but my choice would be perioperative systemic therapy for urothelial cancer, because there are a lot of new potential options, but no new clear standards yet, and some conflicting evidence. Hence, there is a lot to discuss on this topic.
Treatment intensification in mHSPC is also a hot topic right now because there are so many new treatment options. It is not yet clear who needs triplet therapy, and it is also not yet clear if there are patients for whom we can de-intensify treatment.
Lastly, the topic of tailored treatment in kidney cancer. It is important for less frequent forms of RCC including non-clear cell RCC or for hereditary kidney cancer. For ccmRCC there are many possible first line options and it is important to look at how to best select patients.
What are your top three personal highlights of the programme?
Prof. Gillessen: There are many good sessions, but my personal highlights are: Firstly, Plenary Session 3: New strategies in bladder cancer, which will include many interesting discussions on urinary markers, bladder preservation strategies, molecular subtyping and selecting optimal candidates for adjuvant therapy (this is a big open question).
Another highlight is Plenary Session 5: New trials results, which will offer short, concise updates about the most important trials in the field critically discussed by a specialist. It is always interesting to have a critical view on important, practice changing data.
There is a great opportunity to have specialists from different disciplines discuss complex cases in Plenary Session 10: Multidisciplinary sessions for aggressive prostate cancer.
- How to join EMUC22
You can register now to participate in EMUC22 here. For the complete scientific programme, please click here. - ESUI22
The 10th meeting of the EAU Section of Urological Imaging (ESUI22) will take place on the 10th of November in conjunction with EMUC22. Delegates can expect extensive assessments of technological applications in imagine-guiding approaches. ESUI22 will also investigate how imaging enhances urological diagnostics and intraoperative visualisation, and helps define the standardisation of the reporting of urological cancers.
The post EMUC22 Preview: “Treatment intensification in mHSPC is a hot topic right now” appeared first on EMUC25.
]]>The post EMUC22: Relevant topics and Prof. Stenzl’s personal highlights appeared first on EMUC25.
]]>In this article Prof. Arnulf Stenzl (DE), who is one of EMUC22’s esteemed Steering Committee members and the EAU Adjunct Secretary General – Executive Member Science, offers a preview of the most relevant topics at the congress, as well as, his personal EMUC22 highlights.
What are the most relevant topics at EMUC22 and why?
Prof. Stenzl: As a large part of our practice is early detection of prostate cancer, Plenary Session 1: New tools for meaningful questions in early-stage prostate cancer will provide crucial insights into clinically meaningful methods. The session will deliver varying perspectives on whether MRI-targeted and systematic biopsies are still the roadmap for therapy. The delegates will learn how the teamwork among radiologist, a urologist, radiation oncologist and a focal therapist can be the best way in treating patients. In addition, there will be a deliberation on whether or not PSMA (prostate-specific membrane antigen) with MRI is the treatment guide algorithm in high-risk prostate cancer.
The same goes for early detection and monitoring of bladder cancer. Urinary markers will be a topic favourite. During Plenary Session 3: New strategies in bladder cancer, experts will discuss the role of urinary markers in non-muscle invasive bladder cancer; transurethral tumour removal for bladder preservation strategies; molecular subtyping and gene profiling.
Other important topics that EMUC22 will cover are testicular and penile cancers. These rare cancers affect young and usually otherwise healthy men. Fortunately, in most cases, testicular cancer is curable but we must be aware of the long-term physiological and psychological effects of the treatment. Penile cancer is an orphan tumour with mostly unsuccessful treatment options. Plenary Session 8: Interdisciplinary challenges in penile and testicular cancer will comprise of multidisciplinary case discussions with potentially promising options.
What are your top 3 personal highlights of the EMUC22 programme and why?
Prof. Stenzl: My personal highlights include the:
- Interactive case-based debates because these show the real-life challenges faced and strategies undertaken in the clinical practice
- Presentation about artificial intelligence (AI) and on how AI can be used for better and faster exploitation of literature such as “Sense-mining the Literature: How Artificial Intelligence Can Help Us Master the Evidence”
- Presentation on what can uro-oncologists learn with regards to motivation during the most extreme situations in surgery and oncology by a renowned free climber.
To know more about EMUC22, please explore the congress’ scientific programme now.
EMUC22 will take place from 10 to 13 November 2022 in Budapest, Hungary in conjunction with the 10th Meeting on the EAU Section on Urological Imaging (ESUI22).
Interested in presenting at the congress? Submit your abstract(s) before 1 August 2022 (23:59 CEST) for the opportunity for your research to be part of the EMUC22 stellar scientific programme. Click here for more information.
The post EMUC22: Relevant topics and Prof. Stenzl’s personal highlights appeared first on EMUC25.
]]>The post Personalised approaches to treating GU cancers appeared first on EMUC25.
]]>Prof. Lars Dyrskjøt (DK) opened the session with his presentation “Circulating tumour DNA for decision-making in high-risk and metastatic bladder cancer.” He first gave his audience a quick refresher on ctDNA. “Mutated DNA from cancer cells is shredded into circulation. This is named ctDNA, and we can use it as a very sensitive and specific biomarker for tumour burden and metastatic spread.”
“ctDNA has the potential to be used throughout the disease course in patients with cancer,” Prof. Dyrskjøt stated. “We can use it for risk assessment before treatment and cystectomy, as a profiling tool for prognostication, for early diagnosis of minimal residual disease after radical cystectomy, and to monitor treatment response during, for instance, chemo- and immunotherapy.”
Prof. Dyrskjøt mentioned the results from a prospective study he worked on to support these statements. For instance, ctDNA-negative patients were associated with good outcomes – and the other way around. “It is a highly prognostic factor to be ctDNA-positive. ctDNA is highly correlated to disease outcome,” he said, referring to the slide below.
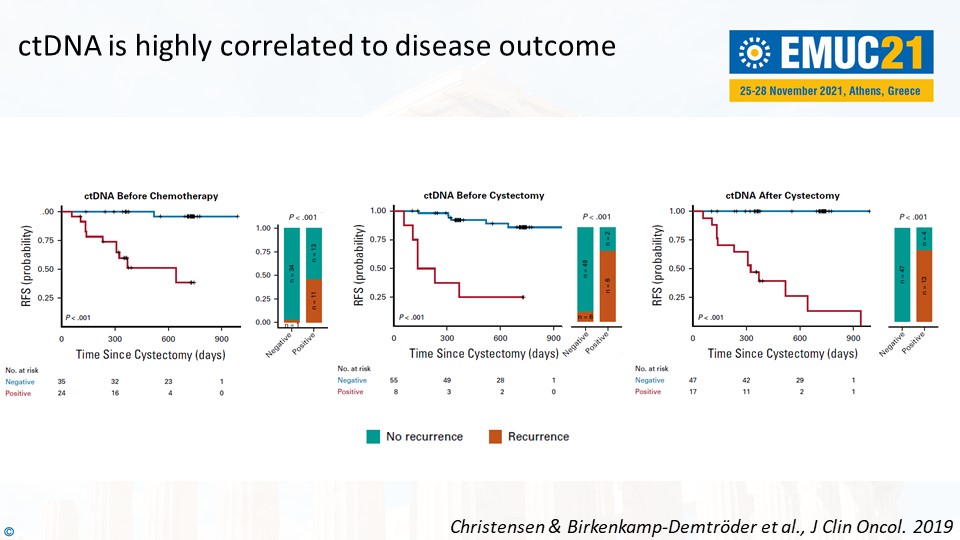
Prof. Dyrskjøt concluded, “What we need to demonstrate now is the clinical impact of ctDNA-based guidance. Can it improve the overall survival? Can it improve the quality of life? Can we reduce costs?”
Practical tips on genetic testing in prostate cancer
In the following presentation, Dr. Elena Castro (ES) gave practical tips on genetic testing in prostate cancer to the attending delegates. “We should consider assessing the HR status early, because it may take some time to retrieve blocks or to consider a re-biopsy. It’s good to know that the BRCA1/2 mutations rarely change status over time. Poly (ADP-ribose) polymerase inhibitors are currently approved after progression to androgen receptor signalling inhibitors (ARSis).”
“Finally, we should offer germline testing to all patients with metastatic prostate cancer. Somatic tests are not validated for germline assessment. We shouldn’t forget to exclude the potential germline origin of the mutations in the cancer-related genes from tumour analyses.”
The other two lectures in Plenary Session 8 were presented by Dr. Maria Rosaria Raspollini (IT) and Prof. Francesco Ceci (IT). (Re)watch all presentations of Plenary Session 8 as webcasts in the EMUC21 Resource Centre. EMUC21 delegates can access all scientific content here. All presentations, full-text abstracts, and (e-)posters are easily accessible in the Resource Centre.
The post Personalised approaches to treating GU cancers appeared first on EMUC25.
]]>The post Trial updates: NIMBUS, FLAME and IMvigor130 appeared first on EMUC25.
]]>NIMBUS
During his presentation “NIMBUS trial – follow up”, speaker Prof. Dr. Marc-Oliver Grimm (DE) provided the trial’s findings. He stated that in high-grade non-muscle-invasive bladder cancer (NMIBC), a reduced frequency of Bacillus Calmette-Guerin (BCG) instillations during induction and maintenance is inferior to the standard BCG schedule regarding time-to-first-recurrence. Particularly, more early recurrences occurred in the experimental arm suggesting inferior efficacy of the reduced-frequency BCG induction schedule.
According to Prof. Grimm, fewer patients were affected with fewer adverse events (AEs) in the reduced frequency arm. He added that NIMBUS is the first prospective trial using routine repeat transurethral resection (reTUR) prior to BCG induction, which was performed in 90% of the patients. The low recurrence and progression rate in the standard frequency arm in a high-grade NMIBC population with an estimated recurrence rate of 21% after three years, and a progression rate of 3.8% at first recurrence may be attributed to the routine use of reTUR.
Further exploring the topic, Prof. Dr. Axel Merseburger (DE) shared points of discussion such as how to identify early recurrent patients; he mentioned biomarkers, which had been discussed during the congress yesterday. If alterations are there, he stated to opt for IO/fibroblast growth factor receptor (FGFR) treatment. In addition, Prof. Merseburger inquired if fewer AEs in the reduced frequency arm are clinically meaningful.
He concluded, “My biggest take-home message from the NIMBUS trial is to use routine reTUR prior to BCG induction and ask a pathologist to see the muscle in the specimen.”
FLAME
Launching the presentations on the FLAME trial, oncologist Dr. Linda Kerkmeijer (NL) stated, “The FLAME trial is the first randomised trial to show that isotoxic focal radiotherapy boosting works. A five-year biochemical disease-free survival (bDFS) of 92% was achieved in mainly high-risk prostate cancer population. The focal boost had no impact on toxicity or quality of life. In addition, the radiotherapy was performed with conventional techniques and at no additional costs.”
In a complementary lecture, discussant radiotherapist Dr. Bradley Pieters (NL) focused on androgen deprivation therapy (ADT), which was used in the study, and on the duration of treatment. He stated, “There will still be discussions with regard to the need for and duration of ADT in very-high-dose-escalated radiotherapy. It’s something to explore further in the future. Another topic that will be investigated is the possibility of safely reducing treatment time and still provide very high doses through Stereotactic body radiation therapy (SBRT), brachytherapy or both.”
IMvigor130
Speaker oncologist Prof. Dr. Aristotelis Bamias (GR) shared some of the key points of the IMvigor130 trial. He stated, “The trial produces valuable information on the role of checkpoint inhibitors (CPIs) in the modern treatment paradigm in advanced urothelial cancer (aUC). Progression-free survival (PFS) is significantly prolonged by the addition of atezolizumab to first-line, platinum-based chemotherapy.”
He added that the current label of atezolizumab monotherapy in first-line treatment is justified and that the role of platinum compound in the context of immunotherapy needs to be further studied. “The evolving results of IMvigor 130 need to be viewed in the context of rapid changes in the treatment paradigm of aUC,” Prof. Bamias concluded.
Discover what oncologist Prof. Dr. Thomas Powles (GB) shared about the IMvigor130 trial, as well as, the full presentations today on the NIMBUS, FLAME, and IMvigor130 trials in the Resource Centre. You can also access vital updates from the CLEAR and Extended vs limited Pelvic Lymph node dissection in prostate cancer trials in the Resource Centre.
The post Trial updates: NIMBUS, FLAME and IMvigor130 appeared first on EMUC25.
]]>The post Bladder-preserving strategies unveiled: Topical therapy and TURBT appeared first on EMUC25.
]]>After Prof. Paolo Gontero (IT) and Dr. Gianluca Giannarini (IT) had given their respective presentations on the use of biomarkers and innovative approaches, Prof. Alfred Witjes (NL) lent his expertise to answer the question of how topical therapy could be improved for bladder preservation in patients with NMIBC.
“Apply proper standard instillation principles, like dehydration and the use of correct doses and frequencies,” Prof. Witjes said. “Electro-Motive Drug Administration (EMDA) and conductive chemo-hyperthermia will certainly improve the efficacy to some extent. Radiofrequency-induced chemo-hyperthermia works and is supported by most data.”
He went on to give his vision of the future: “The Gemcitabine-Releasing Intravesical System looks interesting, but several studies into this are still ongoing. As for thermosensitive gel and liposomes, we are not there yet for NMIBC – but keep your eyes open. With regard to combination therapy, docetaxel for Bacillus Calmette-Guerin-naïve NMIBC looks promising. New forms of immunotherapy combined with intravesical therapy are under investigation.”
How to perform a high-quality TURBT
Prof. Athanasios Papatsoris (GR) gave a lecture on how to perform a transurethral resection of a bladder tumour (TURBT) of a quality as high as possible, referencing numerous studies throughout his presentation. One of them offered a “TURBT checklist,” which Prof. Papatsoris showed with his two slides below.
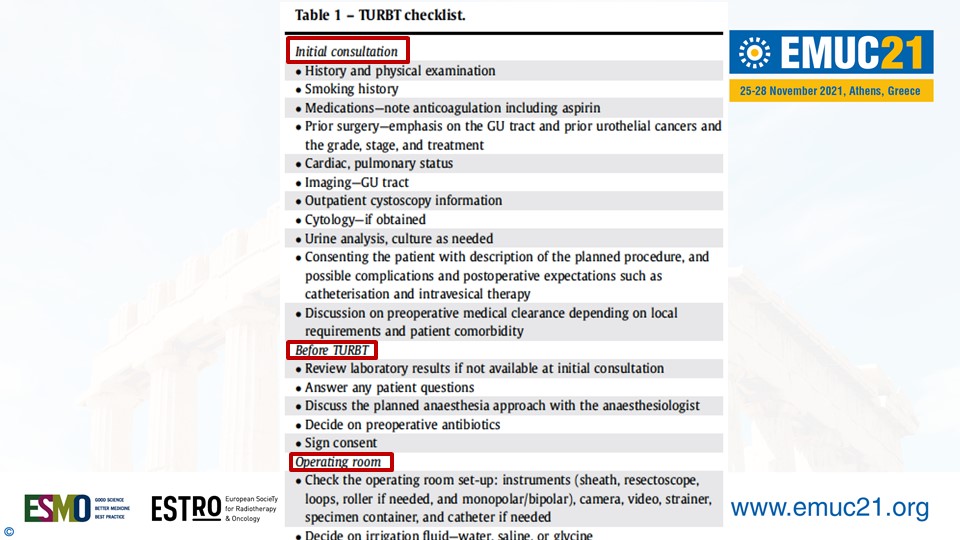
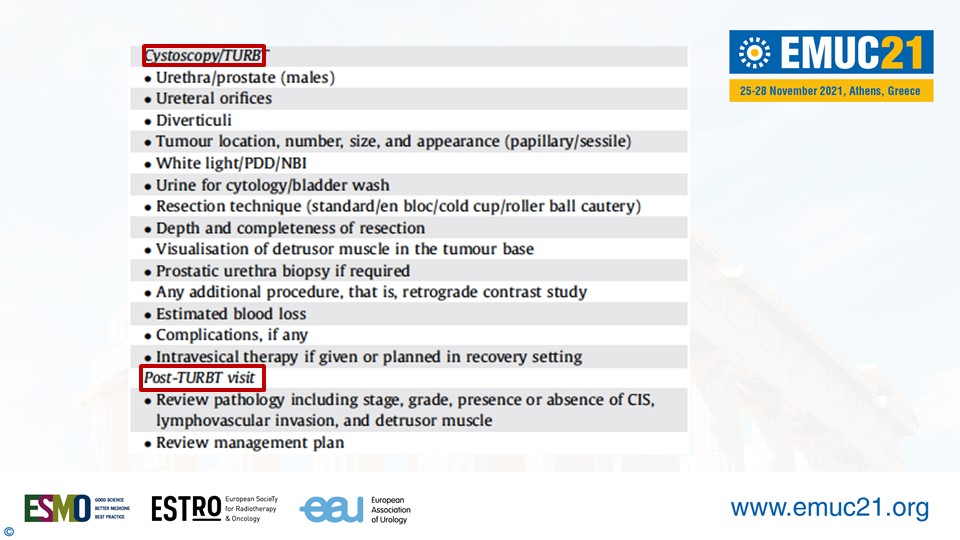
“Attention to detail and a permissive set-up are crucial to an effective TURBT,” Prof. Papatsoris explained. “We need to standardise the technique and learning curve for en-bloc TURBT. En-bloc TURBT has many potential pros, such as tumour sampling in a single piece, shortening of the procedure time and hospitalisation, and the relative reduction of complications and the need for re-TURBT. However, pathologists are not familiar with en-bloc TURBT yet and there is no consensus on the resection tool and energy source yet.”
Prof. Papatsoris ended his presentation putting the spotlight on a procedure that could combine the best of two tools, namely external beam radiotherapy (ERBT) and en-bloc TURBT. “In theory, optical molecular imaging-assisted en-bloc tumour resection integrates the advantages of both and is expected to improve the quality and completeness of transurethral tumour resection, and ultimately improve the oncological outcomes of patients with NMIBC,” Prof. Papatsoris quoted from a study in Frontiers in Oncology. “There are studies underway assessing the combination of en-bloc TURBT and molecular imaging.”
(Re)watch Prof. Papatsoris’ and Prof. Witjes’ full presentations in the EMUC21 Resource Centre. EMUC21 delegates can access all scientific content here. All presentations, full-text abstracts, and (e-)posters will become easily accessible here throughout the congress.
The post Bladder-preserving strategies unveiled: Topical therapy and TURBT appeared first on EMUC25.
]]>The post ESUP Symposium examines the potential of liquid biopsies in uro-oncology appeared first on EMUC25.
]]>The symposium is co-organised by the EAU Sections of Uro-Pathology (ESUP) and Urological Research (ESUR) and the Uropathology Working Group of the European Society of Pathology. Expert speakers were drawn from these bodies, with speakers of a variety of pathology-related backgrounds.
This year, the ESUP Symposium examined the current state of liquid biopsies in uro-oncology, and it possible future applications. What emerged over the course of the afternoon was a future with a promising perspective, but still a lot of work to be done for researchers and pathologists.
Dr. Michelangelo Fiorentino (Bologna, IT), a clinical pathologist, gave an introductory talk on the current applications, and what uro-oncologists should know before using them. Liquid biopsies refers to the use of blood and other bodily fluids as an alternative to tissue samples for diagnostic purposes.
The potential of liquid biopsies is significant, according to Fiorentino: “The major advantages are the non-invasiveness, removing the need for biopsies. Also, liquid biopsies can give a better representation of all the tumour profiles and genetic mutations. Finally, liquid biopsies can give a better indication on the extent of tumour burden.”
In theory, any lab test for tissue can be used to analyse liquids, but they have to be adapted for much lower concentrations of tumour cells. Some tests can require up to 80ml of blood. As it stands, liquid biopsy is currently much more expensive than conventional histology. The reliability of diagnostic accuracy is also inferior. It is also not entirely clear which professional should be in charge of liquid biopsies: pathologists, biochemists, geneticists or (uro-)oncologists.
Potential for BCa
Following talks on kidney cancer (by ESUR Chairwoman Prof. Kerstin Junker, pictured) and prostate cancer and the potential suitability of liquid biopsies for those urological cancers, Prof. Thomas Gevaert (Leuven, BE) spoke on bladder cancer. “In contrast to other urological cancers, BCa has advantage: we can look at blood as well as urine. By combining analysis of the liquids, and with a variety of techniques we can investigate different substances.”
“The majority of patients with metastatic BCa have circulating tumour DNA. This means there is potential value to stratify patients for clinical trials, as well as potential value in diagnostic and follow-up flowcharts. cfDNA/ctDNA is a very sensitive tool to detect early recurrence and minimal residual disease.”
Gevaert postulated that by combining analysis of cfDNA (mutational landscape) and CTC’s (protein expresession), these could be complementary tools with even better results.
Despite aforementioned advantages of liquid biopsies, particularly for BCa, like its non-invasiveness, the combination of urine and blood, and the pre-screening and monitoring, Gevaert pointed out certain hurdles that need to be cleared before liquid biopsies are adopted.
“As with many new techniques, we are still waiting for prospective validation. We also need standardization in our approach. Crucially, we should not be using liquid biopsies unless there is a clear superiority when compared to traditional biopsies. Sensitivity and specificity of liquid biopsies also need to be determined.”
The post ESUP Symposium examines the potential of liquid biopsies in uro-oncology appeared first on EMUC25.
]]>