The post “If you can’t measure it, you can’t improve it” appeared first on EMUC25.
]]>Mr. Leigh: “We will consider three cases in this session, using the format of an M&M Meeting. We will try to be candid and fair, looking for ways to improve practice. We asked our presenters to choose cases from which lessons may be learned. None of the cases have obvious negligence, but all present learning opportunities.”
A quality audit – measuring outcomes and complications
Asst. Prof. Giorgio Gandaglia (IT) presented a prostate cancer case from his institution for review.
- A 72-year-old male
- BMI 23
- Type 2 DM
- Medication: metformin
- PSA 4.3 ng/ml
- CT scan: prostate x 1.5, suspicious module right side, prostate 40ml; adenoma 20 ml, prostate biopsy showed adenocarcinoma of the prostate, FF2, 5/15 positive cores, bone scan was negative, abdominal TC: bilateral renal cysts
The patient underwent a robot-assisted radical prostatectomy. He was discharged on day three postoperative, but on day six, he was admitted to the ER with haematuria and fever, a malfunctioning of the bladder catheter. He was re-admitted to the ER on day 30 with the same complication.
Is it important to chase complications after robotic surgery? According to Asst. Prof. Gandaglia, a wide heterogeneity exists in the rate of postoperative complications after robotic surgery. Although, there has been an exponential increase in the papers using the Clavien-Dondo system over the last few years, only 65% of urologic manuscripts adopt the score correctly.
Asst. Prof. Gandaglia shared details on how his institution learnt from this experience. “The first phase of our prospective study consisted of an audit and feedback process, where the most frequent complications observed in our series were prospectively collected, and in January 2018 an appraisal was done. The most common complication was anastomotic leaks (6.7%). Changes in the surgical technique were proposed to improve outcomes after collegial discussion and review of the surgical videos were recorded during the audit and feedback phase.”
According to Asst. Prof. Gandaglia, the outcome was the introduction of a novel technique for vesico-urethral anastomosis. “The awareness of postoperative outcomes led to the implementation of changes in the surgical techniques that significantly reduced the risk of specific postoperative complications.”
Risks of radical cystectomy
Dr. Carmen Mir (ES) presented a bladder cancer case and how the outcome led to learning and making changes to limit the chance of surgical site infections. She stated that reviewing the risks of radical cystectomy need to cover interoperative, in-hospital, early recovery, and long term. Changes implemented in her institution from this case included fragility assessment for patients over 70 years old, redoes antibiotic therapy and the use of chlorhexidine for prepping. “We also change the surgical instrument set at closure, use running 5mm 1-0 resorbable elastic monofilament, and saline for wound clean up before skin closure”.
A take-home message from Dr. Mir was “Look at your own institution and see what is working and what’s not working. There are a lot of small things that could make a difference to the outcome”.
A need for anticoagulation therapy (ACT) pre-operatively?
Prof. Faiz Mumtas (GB) presented a complicated kidney cancer case of an 80-year-old male with a high BMI of 38 and a visible haematuria with a normal MSU, blood profile and cystoscopy. He had a permanent pacemaker for asymptomatic bradycardia.
According to Prof. Mumtas, in the patients initial CT scan he had a level 2 Pt3b caval tumour. “His staging CT and MRV (Magnetic Resonance Venography) got delayed whilst waiting for a cystoscopy and so he represented with a saddle pulmonary embolism (PE) with an extension in the caval tumour height. With extensive PE we did anticoagulated therapeutically with no significant haemodynamic improvement. Surgery was delayed due to recurrent PE. This further delay led to the growth of the tumour size and it now approached the level of the hepatic veins making it level 3. This indicated a significant progression.”
Prof. Mumtas stated that a cardiac bypass had to be performed at a different institution. He concluded his presentations with the learning points from this case:
- Anticoagulation in the presence of high-risk factors – recurrent VTE (venous thromboembolism) and bland tumours
- Concerning up-to-date imaging, Prof. Mumtas suggests no more than a couple of days before surgery.
- Further multicentre studies are needed to explore the role of pre-operative anticoagulation and neoadjuvant systemic treatments.
- Operating on level 3 tumours only in facilities where cardiac bypass is available, is to manage patients who become haemodynamically unstable with supra-hepatic clamp.
You can watch a webcast recording of the full presentations on the EMUC23 Resource Centre.
The post “If you can’t measure it, you can’t improve it” appeared first on EMUC25.
]]>The post ESUP: A review of biomarkers and molecular tests in bladder urothelial carcinoma appeared first on EMUC25.
]]>Taking place on day one of EMUC23 in Marseille, the symposium was co-chaired by Prof. Maurizio Colecchia (IT), Prof. Kerstin Junker (DE) and Dr. Gladell Paner (US).
Dr. Markus Eckstein (DE) presented his lecture ‘Molecular differences between primary bladder tumours and metastasis and differences in PDL – 1 expression’. He began by explaining the metastatic evolution from stem(s) to branches. “Tumour properties driving clonal evolution include genetic alterations, cell cycle alterations, DNA-repair alterations, cell mortality and EMT/MET.”
He stated that metabolic effects include the environment such as oxygen, nutrients and hormones. Immunological selection pressure includes immune invasion and immune suppression. Niche properties include nutrient/oxygen supply, immune surveillance (liver, brain and bone), and stroma conditions.
With this highly complex interaction between many cell populations and environmental factors, Prof. Eckstein concluded with the question, “Can we go on testing biomarkers in primary tumours for precision oncology?”
Middle-grade NMIBC?
A case study was shared by pathologist Prof. Colecchia (IT) during his lecture ‘Proposal of a new grading in non-muscle invasive bladder cancer’. He took a deep dive into explaining how the grading recommendations for NMIBC could be improved, as well as the reproducibility of the grading system.
Prof. Colecchia sited several studies that tried to correlate outcomes between heterogeneous grades. “There were different thresholds for the fraction of high-grade cells. If it is a <10% of a high-grade tumour cell, there was no change in clinical outcomes of low-grade carcinoma. Distinction between low-risk and intermediate-to-high-risk carcinoma can provide the basis for adjuvant intravesical instillation and regimen of BCG (Bacillus Calmette-Guerin) [with its significant side effects].”
Prof. Colecchia reported that in 2022, the WHO proposed criteria for reporting papillary tumours as high-grade as long as the high-grade component represents >5% of the tumour. Moreover, tumours with <5% high-grade component should be reported as ‘low-grade with <5% high-grade component’.
To watch the full presentation, visit the EMUC23 Resource Centre.
The post ESUP: A review of biomarkers and molecular tests in bladder urothelial carcinoma appeared first on EMUC25.
]]>The post EMUC23: GU cancer game-changers for 2023 appeared first on EMUC25.
]]>Collaborative efforts are required to drive game-changing advancements in medical research and patient care. The upcoming 15th European Multidisciplinary Congress on Urological Cancers (EMUC23) is the perfect platform to showcase and review important GU cancer trial results and new technologies.
Plenary Session 7 on day three (Saturday, 4 November, 08:45 – 10:05) of EMUC23 will feature clinical trial presentations and multidisciplinary discussions. This “Game-changing session” will be chaired by Prof. Axel Merseburger (DE), radiotherapist Prof. Valerie Fonteyne (BE) and medical oncologist Prof. Karim Fizazi (FR).
Merseburger: “Multidisciplinary meetings in onco-urology play a pivotal role in fostering collaboration among various medical specialists dedicated to the care of GU cancer patients. The EMUC Congress excels in bringing together experts from diverse fields such as medical oncology, radiation oncology, surgical oncology, pathology, nuclear medicine, urology, and radiology. This inclusive approach cannot be overstated, as it facilitates a comprehensive and holistic evaluation of complex cases and clinical trial presentations”.
“Each specialist contributes unique insights based on their expertise, allowing for a thorough analysis of treatment options and potential challenges. This collaborative strategy helps prevent tunnel vision. It ensures that all available options, from surgery to radiation to systemic therapies and supportive care, are considered in the context of the patient’s overall well-being.”
GU cancer trials to be discussed at EMUC23
Urologist Prof. Maxine Tran (GB) will present on nephron sparing treatment (NEST) for small renal masses: A feasibility cohort-embedded randomised controlled trial (RCT) comparing percutaneous cryoablation (passing small needles through the skin to freeze the kidney tumour) and robot-assisted partial nephrectomy. This RCT is of significant interest due to the lack of high-level evidence on small renal mass (SRM) management, with previous classical RCTs failing to meet accrual targets.
Prof. Stephen Freedland (US) will share the latest progress on the phase 3 EMBARK trial, whereby trial data has shown that adding enzalutamide to leuprolide cuts the risk of metastasis or death by 50% in patients.
Prof. Merseburger: “This is a hot topic right now as the FDA granted priority review of enzalutamide for nmCSPC with high-risk biochemical recurrence. The FDA decision is expected in Q4 of this year for the new drug application that has been supported by data from this phase 3 EMBARK trial. Discussion remains on the value of PSMA-PET in this situation.”
Medical oncologist Dr. Yohann Loriot (FR) will present details on the THOR study reinforcing the activity of erdafitinib as personalised therapy for metastatic urothelial patients with FGFR mutations. Erdafitinib is included in the current EAU bladder cancer guidelines. The THOR study leads to precision medicine in advanced bladder cancer for 3rd line treatment for patients with EGFR alterations. All metastatic urothelial patients should be tested for FGFR3/2 alterations.
Other trial results that will be presented and discussed by the multidisciplinary panel include TALAPRO-2 and PROpel, as well as an update on PSMA targeting.
Uniting medical experts for innovation and progress
The EMUC23 congress is a collaboration of the European Society for Medical Oncology (ESMO), the European SocieTy for Radiotherapy and Oncology (ESTRO) and the European Association of Urology (EAU). Other sessions that will take place in conjunction with EMUC23 include the EMUC Symposium on Genitourinary Pathology and Molecular Diagnostics (ESUP), the Meeting of the EAU Section of Urological Imaging (ESUI), European School of Urology (ESU courses and Hands-on Training) and the Young Academic Urologists Meeting (YAU).
If you register by 19 October (23:59 CEST) you will benefit from some registration savings. Don’t miss your opportunity to participate within this collaborative learning environment! Browse the full scientific programme.
The post EMUC23: GU cancer game-changers for 2023 appeared first on EMUC25.
]]>The post Synergy of specialties at EMUC23: Why MDTs are paramount to optimal patient care appeared first on EMUC25.
]]>As always, the scientific programme of the upcoming 15th edition (EMUC23) will reflect the interdisciplinary approach in the treatment of genitourinary (GU) cancers but will have new features. This article offers information on the latter, the value of a multidisciplinary team (MDT), and viewpoints from some of the distinguished members of the EMUC Steering and Scientific Committees.
New and improved programme
To further solidify the multidisciplinary nature of the congress, the meeting of EAU Section of Urological Imaging (ESUI) will merge with the congress. Crucial updates such as the latest evidence in imaging trials and their clinical implications; unmet needs in uro-oncology imaging; other imaging modalities, and more will kickstart EMUC23 on 2 November 2023.

The ESUI meeting will merge with this year’s EMUC23 programme.
In addition, one of the most popular features of the scientific programme, the Multidisciplinary Case Discussions, will be more data-driven, infused with robust statistics, and delivered in an improved structured format.
To enrich the EMUC23 experience, the exhibition will also be a must-visit element of the congress showcasing innovations in equipment, scientific publishing, and pharmaceuticals.
EMUC23 and nuclear medicine
Prof. Daniela Oprea-Lager (NL) stated that attending EMUC23 will not only be beneficial to her fellow nuclear medicine physicians, but to other healthcare professionals as well. “The congress will deliver novel developments from the preclinical to the clinical levels of interest. EMUC23 will be a platform where various perspectives are offered and topics on imaging are adequately integrated during the patient case discussions. Experts from diverse fields will brainstorm and deliberate to improve clinical practice and to avoid futile treatments in categories of patients who might not respond to therapy.”
Prof. Oprea-Lager shared that her favourite EMUC sessions are the Multidisciplinary Case Discussions and Game Changing sessions, where interdisciplinary collaboration will be at its pinnacle. She said, “Generally, there are various possibilities when treating certain patients. The key is selecting the most appropriate approach, capitalising the benefit, and minimising the adverse effects and costs.”
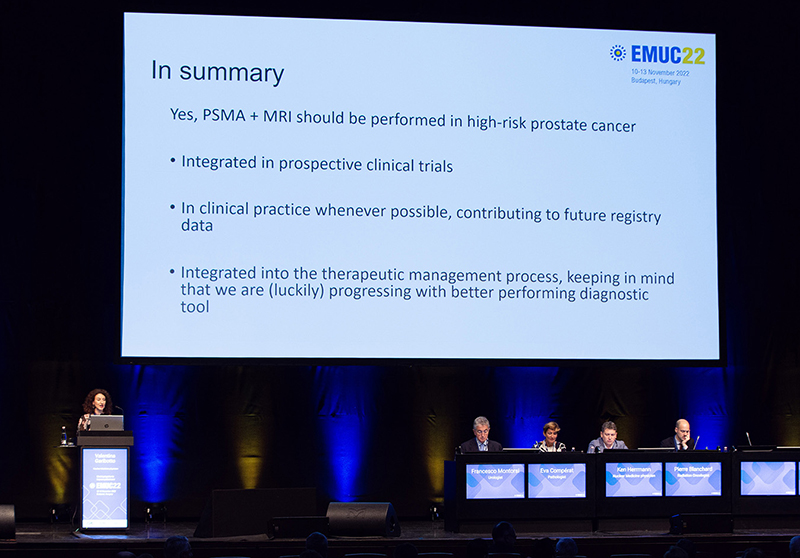
During EMUC22, nuclear medicine physician Prof. V. Garibotto (CH) deliberates why PSMA + MRI should guide treatment algorithm in high-risk prostate cancer.
Role in the MDT
“With the implementation of next-generation imaging and the theragnostic concept in clinical practice, the tasks of the imaging doctor became complex. We see what we treat and we treat what we see, but the aims are to position the patient centrally and to act from an individualised perspective,” she said. According to Prof. Oprea-Lager, this is how to carry out these aims:
-
-
-
- Speak the same language with clinical partners
“Imaging doctors, nuclear medicine physicians, and radiologists, need to have the knowledge and high level of expertise to function as equal discussion partners.” - Identify the gaps in daily practice
“Push the limitations and innovate towards answering clinical needs by using imaging tools.” - Be aware of the consequences of “seeing more and treating more”
“Nowadays when we see more, we may upstage/downstage disease and change the initially proposed treatment plan for a still unknown survival benefit. However, the nuclear medicine physician has to possess a good understanding of all factors related to disease history, current medical status, metastatic patterns of urological cancers, pitfalls, and final image interpretation. Once we have these, we can adequately stage/re-stage patients and plan the optimal treatment in dialogue with the clinicians in the MDT and with the patient.” - Adequately select and identify the ideal candidates (i.e. patient categories that may benefit from the proposed treatment)
“Patient selection and response evaluation criteria based on harmonised, repeatable protocols, and adequately performed scans are some of the most challenging tasks of the new-generation imaging doctors.”
- Speak the same language with clinical partners
-
-
Solving dilemmas together
According to Prof. Oprea-Lager, MDT has been implemented in the Netherlands for more than 10 years. However, the presence of radiologists and nuclear medicine physicians in the MDT is a novel element. She explained, “It all began with the need to have all key specialties present in the multidisciplinary process of diagnosis and treatment of patients with urological cancers. Nowadays, specialist diversity is a matter of shared decisions and best-practices approach within the large uro-oncology domain. We are not competing with other disciplines; we try to solve dilemmas together, and successfully translate anatomic and metabolic knowledge into the clinical pathways.”
EMUC23 and medical oncology
“We, medical oncologists, generally focus on advanced disease. Most scientific meetings have sessions that only cover this topic and topics related to it. In contrast, EMUC provides updates and knowledge exchange on various stages of GU cancers. It is during the early stages that plenty of evidence is generated. This can change or will change clinical practice. With this in mind, it is in the best interest of our patients to keep ourselves updated and EMUC can help with that,” said Dr. Elena Castro (ES).
Advantages of MDT
According to Dr. Castro, when the management of GU tumours becomes increasingly complex due to multiple treatment options, a well-coordinated MDT is paramount in pinpointing the most appropriate disease management. She explained, “This is especially true in patient cases with particularities that have more than one potential option and/or when the Guidelines do not currently offer clear recommendations. I personally find MDT discussions very helpful in coming up with the best care possible as the decision is not based on one person’s point of view. Additionally, MDTs are essential in identifying candidates suited for clinical trials as they could benefit from treatments not yet widely available.”

Urologist Dr. T. Kuusk (GB) presents a case on adjuvant treatments and recurrent disease during the Multidisciplinary Case Discussion session on kidney cancer at last year’s EMUC.
Dr. Castro shared that in her practice, most GU patients with localised disease who benefit from localised treatment or even surveillance, are usually managed by urologists or radiation oncologists. However, there are some cases that may require neoadjuvant or adjuvant systemic treatment. Thus, coordination between surgeons and medical oncologists is key.
Patients with (recurrent) metastatic disease are usually referred to the medical oncologist. Concerning prostate cancer, some patients with metastatic disease are managed by urologists or radiation oncologists. These patients are then referred to the medical oncologists after progression to the initial therapy or if the most appropriate treatment requires chemotherapy or other systemic treatments.
Spain’s take on MDT
“If not in all, in most tertiary hospitals in Spain, MDTs are the common way to manage cancer patients for GU tumours and most tumours. The composition of the MDTs may vary depending on the specialists that are relevant for a particular tumour type, but MDTs typically include surgeons, medical oncologists, radiation oncologists, pathologists, and radiologists. For instance, for prostate cancer, it is important that the nuclear medicine specialists are also involved,” stated Dr. Castro.
MDT becoming compulsory?
According to EAU Secretary General and EMUC Steering Committee member, Prof. Arnulf Stenzl (AT), an MDT’s involvement in treating onco-urology patients may become imperative in health insurance matters. He stated, “We see insurance companies and authorities in several countries require that onco-urology patients must be seen by a multidisciplinary tumour board to receive reimbursements for a systemic (or new interventional) treatment or diagnosis such as PSMA-related diagnosis or treatment. It would be beneficial if medical specialists become more informed in many aspects of GU cancer treatment beyond the scope of their core specialism.”
| Join us at EMUC23 |
| EMUC23 is an all-encompassing congress designed to enrich your clinical practice and patient care. Explore the congress’ scientific programme to know what’s in store for you. Secure your place at EMUC23 and register now to benefit from the early-fee rates. Don’t miss out! |
The post Synergy of specialties at EMUC23: Why MDTs are paramount to optimal patient care appeared first on EMUC25.
]]>