The post WoodFire® ignites RCC deliberations appeared first on EMUC25.
]]>WoodFire® comprised rapid-fire debates on renal cell carcinoma which abided by the following cardinal rules:
- Data not given here are considered within the limits of normal pathological findings.
- If you want to introduce a patient to a trial, name the trial and objectives. The trial has to be open.
- If you want to treat a patient with systemic therapy, only name one regimen you would prescribe and the dosage.
- Come up with a clear recommendation assuming the patient will choose your option.
- Do not tell what you could do but what you would do.
One of the four cases
Moderator medical oncologist Asst. Prof. Ronan Flippot (FR) kickstarted WoodFire® with the first case: a 40-year-old female patient who had a small abundance of haemoptysis, which prompted a CT scan. A kidney mass biopsy was performed and the results revealed large atypical cells, sometimes fusiform, and eosinophilic cytoplasm. Necrosis was present as well. The markers were identified as CAIX+, CD10+, and PAX 8+.
Pathologist Dr. Soha El Sheikh (GB) stated that PAX 8+ indicates a primary renal tumour rather than a metastasis. CAIX+ and CD10+ are usually seen as positive in clear cell renal cell carcinoma (ccRCC) however the morphology describing fusiform and eosinophilic cytoplasm does not fit the typical low-grade ccRCC profile. Necrosis and the large atypical cells indicate aggressive behaviour. Dr. El Sheikh deduced that it was potentially a high-grade ccRCC. Prof. Flippot revealed it was clear-cell RCC ISUP 4 sarcomatoid.
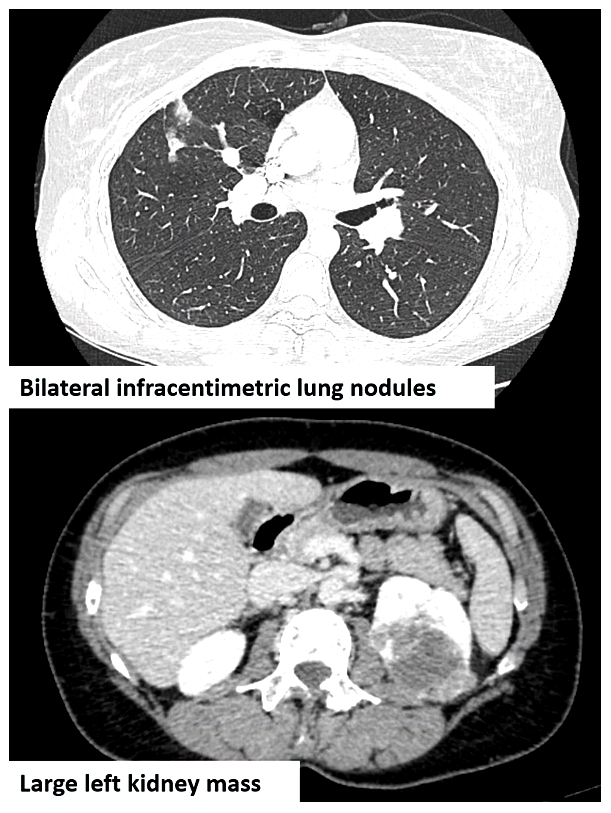
Prof. Flippot proceeded to describe what was seen in the CT scan (see image): primary lung metastasis, a small abundance of haemoptysis, the nodules were in the proximity of major vessels in the lung, and the primary tumour was asymptomatic. He asked the panel if the primary tumour should be removed. Urologist and Chair of Plenary Session 8, Prof. Axel Bex (GB) opted for systemic therapy. Medical oncologist Dr. Laura Marandino (GB), radiation oncologist Prof. Ben Vanneste (NL), and urologist Dr. Wolfgang Loidl (AT) agreed.
Prof. Flippot proceeded with the case and stated that the patient was given pembrolizumab and axitinib. Complete response on metastasis was achieved at six months and the primary tumour was still unresected. However, at 12 months, new metastasis has formed in the lung (one to two confirmed lesions of approximately 8mm). Prof. Flippot asked the panel what the next step is.
Prof. Bex suggested a consultation with a multidisciplinary tumour board. Prof. Vanneste advised to continue with the systemic treatment and perform stereotactic body radiotherapy (SBRT) for the lesions. He expects no toxicity and local control of the lesions can be achieved. Dr. Marandino agreed with opting for continued systemic therapy, followed by an early interval scan to check that there is no further progression before performing stereotactic ablative radiotherapy (SABR).
Prof. Flippot said that indeed SBRT was applied for the lesions and the medications were continued. At three months, there was no recurrence of the disease. At six months, the primary tumour was still intact. Should the tumour be removed? Dr. Loidl replied that it has to be discussed with the patient. Prof. Bex advised to continue with the systemic therapy and have an interval scan. Dr. Marandino agreed with the continued systemic therapy. Prof. Vanneste advised cytoreductive SBRT. He stated, “It’s not a standard procedure. You can avoid the comorbidities of the operation and theoretically, you can also initiate the systemic response with the local treatment.”
Prof. Flippot revealed that a partial nephrectomy was performed on the patient and systemic therapy was stopped. After six months, peritoneal progression was evident. Fortunately, the patient could participate in a clinical trial where she received pembrolizumab and lenvatinib. She had sustained a response even two years later.
About WoodFire®
“WoodFire” was coined to describe the “quick-fire, high-pressure nature” of how Dr. Christopher G. Wood, KCA’s previous Chair of the Board of Directors, light-heartedly spurred on his peers on how to treat patients with kidney cancer.
Discover what the experts say in the other three patient cases. Visit the EMUC24 Resource Centre for the full presentations.
The post WoodFire® ignites RCC deliberations appeared first on EMUC25.
]]>The post EMUC23: What’s new in GU screening? appeared first on EMUC25.
]]>Grounds for RCC screening
“RCC screening is a topic of great interest to patients, clinicians, and policymakers. Fascinating data will come from the Yorkshire Kidney Screening Trial (YKST),” stated urologist Prof. Grant Stewart (GB) during his presentation “Rationale for renal cell carcinoma screening”.
A sub-study of the Yorkshire Lung Screening Trial, the YKST is a targeted screening of high-risk individuals already attending for another screen test. The recruitment of 4,000 participants was completed in October 2022 and the six-month outcome review came out in May 2023. In January 2024, the report will be published.
Prof. Stewart referred to the Wilson and Jungner/WHO screening criteria, which often represent the de facto starting point for screening decisions today. The criteria comprised 10 principles and Prof. Stewart correlated each principle with the current data available for kidney cancer:
- The condition sought should be an important health problem
“In the UK, kidney cancer is the 7th most common cancer wherein 50% of patients die. An increase in the disease’s incidence in the next 10 years is predicted.” - Facilities for diagnosis and treatment should be available.
“There are well-established diagnostic and treatment pathways.” - There should be an accepted treatment for patients with recognised disease.
“The range of options for patients include surgery, ablation, and active surveillance.” - There should be a latent or early symptomatic stage.
“Yes, there is when it comes to small renal cancer but the vast majority is asymptomatic. This is why we need a way of identification.” - The natural history of the condition, including the development from latent to declared disease, should be adequately understood.
“Yes, it is partially as all lethal RCCs start as small cancers. However, currently, it cannot be predicted which small renal cancers will progress.” - There should be a suitable test or examination.
“Yes, ultrasound or LDCT (low-dose nonenhanced computed tomography) is used.” - The test should be acceptable to the population.
“There is apparent patient accessibility.” Prof. Stewart presented the findings of an online survey concerning public attitudes toward screening for kidney cancer regarding the five screening modalities: urine, blood, ultrasound, kidney computed tomography (CT), combined kidney and lung CT. The majority have opted for the combined kidney and lung CT. - There should be an agreed policy on whom to treat patients.
“Yes, there is with all renal mass patients but not necessarily with Sx/TA.” - The cost of case-finding (including diagnosis and treatment of patients diagnosed) should be economically balanced in relation to possible expenditure on medical care as a whole.
“It is theoretically proven for surgery to be more economical when compared to drugs.” - Case-finding should be a continuing process and not a “once and for all” project.
“This is still unknown. Is repeated screening economically viable?”
Interception to prevent urothelial cancer
During the presentation “Large-scale interception using personalised prevention algorithms – an opportunity for urothelial cancer screening”, medical oncologist, Asst. Prof. Ronan Flippot (FR), stated that urothelial cancer is the 6th most common cancer type wherein 25% to 30% is muscle-invasive presentation, and a five-year survival rate (i.e. 70% localised, 40% regional and <10% distant). The disease affects the ageing population (the median age of onset is 75 years) and frail comorbid patients.
According to Prof. Flippot, a large-scale interception programme has the potential to improve bladder cancer screening. Adherence of patients and ambulatory care professionals, and funding are paramount. He underscored that an interception programme can be significant for prospective screening trials and interventional strategies evaluation in multiple-risk settings. Furthermore, the constitution of biobanks will bring value to molecular detection programmes.
To learn more, access the full presentations of Plenary Session 1 through the EMUC23 Resource Centre.
The post EMUC23: What’s new in GU screening? appeared first on EMUC25.
]]>